When new epidemics hit us, calls for infrastructural development are renewed. More investment in hospital facilities, medical staff and the development of effective protocols for disease control is clearly advisable as seen with the recent end of the Ebola outbreak in West Africa. On the other side of the globe, South Korea’s sudden MERS (Middle East Respiratory Syndrome) epidemic in 2015 provides a different picture. What terrified people in South Korea during the seven-month long outbreak was not only the rapid spread of an unfamiliar virus but also the unexpected inability of one of the most high-tech hospitals in Seoul to isolate potentially infected individuals. The country’s most lavish medical establishment, Samsung Medical Center, had spent 10 billion won ($8.9 million) for the renovation of its mega-size emergency room just two years before the MERS outbreak (The Wall Street Journal, 2015/06/18), but it was not prepared to prevent intra-hospital transmission (Ki 2015). The South Korean experience presents an alarming scenario, one in which technical advancement does not guarantee efficient control and prevention. Strengthening infrastructural capacities continues to be the dominant response to various health risks, yet such attempt often underestimates the very important fact that health infrastructures are not the stable material base on which biomedical superstructures rest.
Health infrastructures, rather, are dynamic but fragile networks requiring efficacious connections between human and material resources.
The proliferation of anthropological explorations on various forms of sociomaterial infrastructures, such as electricity, financial mechanisms, power plants, water delivery, roads and media, has vigorously shown the relational and ontological complexity of these established networks (Anand 2011; De Boeck 2011; Larkin 2008;Von Schnitzler 2013). Infrastructure has “effects and affects far beyond their technical functioning” (Fortun and Fortun 2015: 365) and operates “on multiple levels concurrently” (Larkin 2013: 335). Several hospital ethnographies also directly and indirectly affirm these insights, as they unravel how laboratories (Street 2014a), oncology wards (Livingston 2012) and diagnostic procedures (Mol 2002) draw on multiple modes of knowledge and operate through the “relationships between people, stuff, and space” (Street 2014b).
In this short essay, I propose approaching infrastructure from the standpoint of care in order to discern how an assemblage of human bodies and things is made through everyday practice. Our basic experience of health care intuitively suggests a web of complex relations that sustains and intervenes in our bodies. However, an issue less explored is what makes such infrastructural connections reliable and durable. If infrastructures are indeed fragile, unruly and unpredictable assemblages of people and things (Bennett, 2010), what makes such association and alignment possible?
Expanding the notion of care from interpersonal morality to an integrating force might enable better understanding of how to fix infrastructural relations.
In the following, I trace the recent development of dialysis infrastructure in Thailand and explore various attempts to make this new system work for poor patients. Dialysis is by no means a novel technology, but emplacing it as a part of universal health care provision requires a new set of infrastructural connections, an entwinement of political rationality, administrative techniques, material distributions and human resources. By tracing flows and congestions in this nascent network, I focus on the work of care that makes this entanglement happen. In order to replace one’s failing kidney function by an external filtering system, treatment protocols, membranes, catheters, dialysis fluids, and the insurance schemes have to be interlinked and aligned. Then, what is care in this messy network?
Conjuring Dialysis Infrastructure: Peritoneal Dialysis (PD) First Policy in Thailand
Thailand is one of the few developing countries to have a relatively well developed public health care infrastructure, which ensures universal health coverage for all citizens, besides a thriving private health market for global medical tourists. Renal replacement therapy (RRT) for end-stage renal disease is a key policy which demonstrates the comprehensiveness of the Thai universal health coverage scheme, yet it took several years to be incorporated into the insurance package. While antiretroviral treatment for HIV/AIDS patients was introduced in 2004, chronic renal failure patients had to wait four more years to receive free RRT. Unlike HIV/AIDS, kidney diseases have never reached the global or national health agenda, as they are non-communicable, chronic and degenerative. Continuous RRT is life-preserving yet is resource intensive and expensive.
To ensure universal access to RRT, in 2008 the Thai government introduced peritoneal dialysis (PD) as a primary treatment option. While there are two types of dialysis treatment—PD and hemodialysis—used to redress the ongoing effects of kidney failure, the government choice for the adoption of PD first policy was made on the grounds of infrastructural reason. Demand for RRT has rapidly increased in Thailand, yet most of the available hemodialysis machines and trained medical staff were concentrated in urban areas. Without a large amount of investment in rural health care facilities, it was impossible to make hospital-based hemodialysis widely available. For many nephrologists and kidney patients, the PD first policy was debatable because PD, although its long-term cost would not be significantly cheaper than hemodialysis, is more likely to create a higher risk of complication and failure (Pantipa Sakthong and Vijj Kasemsup 2011; Sripen Tantivess et al. 2013; Viroj Tangcharoensathien et al. 2013). Yet, the PD first policy was eventually chosen because it was deemed an easier way for poor patients to obtain dialysis. PD allows patients to conduct self-care in their homes thereby saving on travel costs.
In designing and implementing the PD first policy in Thailand, the guiding principle for the Ministry of Public Health (MOPH) and the National Health Security Office (NHSO) was the cost-effectiveness of the program. Here, two points are crucial to understand this policy agenda. First, the primary aim of universal health coverage is to prevent catastrophic health expenditures among poorer households. In this principle, the accessibility of treatment needs to be more emphasized than the long-term survival of patients. Second, there is an expectation that the pre-existing health infrastructure can facilitate and incorporate this new policy. The MOPH and NHSO encouraged district hospitals to install a PD clinic with the consideration that district hospitals would utilize “comprehensive primary care networks at the subdistrict and community levels” (Sripen Tantivess et al. 2013). District hospitals are expected to create “treatment partnerships with private facilities” (ibid) to deal with patients who are not suitable to receive PD. In an ideal design, there would be a working and well-connected network between district dialysis clinics, upper-level hospitals, private facilities, subdistrict health workers, village health volunteers, and individual patients and their family members. This network is designed to cover patients with various needs, to provide information and education, and to make home care possible.
Missing Link
Ruen, a 38-year-old single Thai man and an end-stage renal failure patient, was desperately waiting for his turn to get dialysis. He was waiting for an appointment with a nephrologist in the provincial hospital to undergo a simple surgery to insert a Tenckhoff catheter in his abdomen. This soft rubber tube is essential to start PD. Through this tube, a cleansing liquid flows into the abdominal cavity, where it is allowed to circulate for several hours collecting waste products from the blood, and is drained off. Ruen was one of the frequent flyers to Ban Phaet Hospital where I conducted dissertation research on universal health coverage between 2010 and 2012, and we spent many hours together during his hospitalization.
Nurse Mim was quite sure that Ruen was eligible to start PD according to the national protocol, but was unable to tell him an exact date. Nurse Mim was the only dialysis nurse in Ban Phaet Hospital. Although the PD first policy was launched in 2008, in Chiang Mai province only a few district hospitals had opened the dialysis clinic, and Ban Phaet Hospital was one pioneering place. Of the 12 patients who Nurse Mim had been treating, Ruen spent the longest time in the ward. Nurse Mim explained to me: “I can manage his case here, if he received catheter insertion. Then, I can teach him how to do dialysis at home and how to take care of himself. But before that, there is nothing I can do for him.”
Under the current PD first policy, patients who seek hemodialysis as first line treatment had to shoulder the costs burden themselves, and Ruen became trapped within this regulation. Without catheter insertion, Ruen could not start his PD. During this prolonged waiting time, his condition worsened, and hemodialysis became the only viable option for him. Ruen received 14 sessions of hemodialysis in the provincial hospital making out-of-pocket payments and reached the point that his family could no longer help him. He had to return to Ban Phaet Hospital where again he was made to wait. Nurse Mim arranged several referrals to the provincial hospital for Ruen, but his case was one of several in a long waiting list.
As it became impossible to predict when Ruen’s turn would come, Nurse Mim found another chance to refer Ruen when she met a nephrologist in a university hospital and learned that he might be able to provide surgery for PD therapy. As a professor in the medical school, he seemed to have more autonomy to choose patients. This time, Nurse Mim contacted the head nurse in the kidney clinic in the university and arranged the referral. With a detailed explanation of the guidelines for end-stage kidney patients, Nurse Mim remarked: “Ruen might get free hemodialysis. If someone is scheduled to receive surgery for peritoneal dialysis, they can have free dialysis for ninety days before the surgery.”
Through Nurse Mim’s meticulous study of rules and investigation of local resources, it seemed that Ruen now had a glimpse of hope.
On the morning of the referral day, Ruen was extremely anxious. He had stopped dialysis for several weeks and his shortness of breath had become much more severe. After we were dropped at the front gate of the university hospital, Ruen’s aunt asked a nurse for a portable oxygen cylinder, and the nurse then sent Ruen to the emergency room. Nurse Mim had told us to go to the kidney clinic directly, yet Ruen was suddenly stuck in the crowded emergency room (ER). In the ER, a group of doctors, medical students and nurses gathered around Ruen and checked his vital signs and started an abdominal ultrasound. After an hour and a half in the ER, a doctor said that Ruen could not go to the kidney clinic that day. The reason provided by this doctor was that Ruen’s condition was too weak to start PD, and it was recommended that he should go to the private clinic first for hemodialysis instead. Ruen’s aunt gently told the ER nurse that she had no money left for hemodialysis. The ER nurse replied in a sympathetic tone: “The patient should have no other symptoms except kidney failure. He needs to be healthy enough to wait a whole day in the clinic.”
This was a deeply frustrating moment for all involved in Ruen’s pursuit of life-saving care. The PD first policy had been of some use to Ruen but at this crucial point the system failed to provide the very treatment that he had desperately waited for. The district hospital nurse followed the treatment guideline, arranged several referrals for further care, sought collaboration with upper level hospitals and consulted with family members. Here, the basic limitation was that medical staff in the district hospital were incapable of providing dialysis treatment by themselves.
In its original design, the district hospital was supposed to work only as a node within the bigger dialysis network, yet without the basic link, the inserted catheter, the circuit of care could not be fully established.
Suturing and Caring
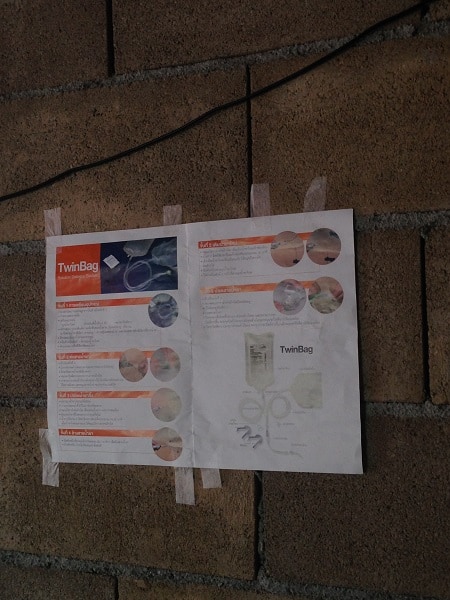
In Thailand, most CAPD (continuous ambulatory peritoneal dialysis) patients use a twin-bag system. (Photo by B.K. Seo)
Fortunately, this is not the end of the story. Nurse Mim continued to pursue Ruen’s case, and the provincial hospital finally accepted the referral. To stabilize his condition, several hemodialysis sessions were offered free of charge. Finally, the catheter was inserted, so he could start PD. When Ruen returned to the district hospital ward for further observation and extra training for home dialysis, I was struck by how thin he was. With all excess water gone, Ruen had lost a significant amount of weight and appeared dangerously frail.
The whole system had been deeply troublesome for Ruen but finally it had delivered a tangible result when the catheter was inserted. Boxes of dialysis solutions manufactured from Baxter’s brand new factory in Bangkok were delivered to the ward straight away, and costs were eventually covered by universal health coverage. The inserted catheter finally allowed Nurse Mim to deliver appropriate care. She taught Ruen the basic procedure and skills for home care including sanitizing the devices, changing syringes, measuring the fluid and detecting problems. After all, it was essential that Ruen would be able to carry out PD at home.
The promise of free access to dialysis was eventually realized, but the journey to get there had been absolutely exhausting. Ruen’s experience signifies both the successes and failures of the universal dialysis policy. PD first policy was designed for patients who could not afford privatized hemodialysis treatment, and Ruen was part of the target group for this newly established program. Here, the problem was not the absence or breakdown of the treatment infrastructure. Instead, it was a matter of adjusting. In this already overburdened system, the medical staff had to constantly tussle with unpredictable and restrictive bureaucratic and institutional conditions of dialysis to make efficacious connections between the patient and the upper-level medical institutions. Without this basic suturing, life-sustaining care would not have been possible.
In Ruen’s irksome pursuit of treatment, care was dispensed at multiple levels. It is important to note that Ruen’s patience and endurance drove others to care for him and drew ethical responses (Seo 2016). Yet, Nurse Mim’s administering of care was not without obstacles. As a node within the larger dialysis infrastructure, the crucial role given to Nurse Mim was to probe fragile institutional networks. Here, the efficacy of dialysis infrastructure largely relies on human effort. As the regular filtering finally becomes possible through the connection between the catheter inside Ruen’s abdomen and the Y-shape transfusion syringe attached to dialysis solution and drainage bags, Nurse Mim’s presence may become less prominent. Yet, this whole set of technical connections is an accomplishment of care.
To initiate, repair and sustain this life-sustaining association, caregiving has to be infrastructural in a sense that it requires an assemblage of ethical, technological, institutional and bureaucratic practices.
If we approach health infrastructure as a generative ingredient of caregiving, it also changes how we approach forms of care. Infrastructural relations are “lines not of flight, but of interaction” (Ingold 2011:63), and the ongoing task is how to suture and interweave various materialities and uncertainties. In this dynamic, the form of care is not bound to the division between the macro and the micro, the moral and technical, or between the medical and familial, but has to be open to all possible associations and convocations. Health infrastructure is both an object of inquiry and an ontological vantage point from which to explore the assembled nature of care.
Co-published by Allegra Lab and the Collaborative Blog Medizinethnologie: Body, Health and Healing in an Interconnected World
References
Anand, Nikhil. 2011. Pressure: The PoliTechnics of Water Supply in Mumbai. Cultural Anthropology 26, no. 4: 542-564.
Bennett, Jane. 2010. Vibrant Matter: A Political Ecology of Things. Durham: Duke University Press.
De Boeck, Filip. 2011. Inhabiting Ocular Ground: Kinshasa’s Future in the Light of Congo’s Spectral Urban Politics. Cultural Anthropology 26, no. 2: 263–286.
Fortun, Kim and Mike Fortun. 2015. An Infrastructural Moment in the Human Sciences. Cultural Anthropology 30, no.3: 359-367.
Ingold, Tim. 2011. Being Alive: Essays on Movement, Knowledge and Description. London: Routledge.
Ki, Moran. 2015. 2015 MERS Outbreak in Korea: Hospital-to-hospital Transmission. Epidemiology and Health 37:e2015033. doi:10.4178/epih/e2015033.
Larkin, Brian. 2008. Signal and Noise: Media, Infrastructure, and Urban Culture in Nigeria. Durham: Duke University Press.
Larkin, Brian. 2013. “The Politics and Poetics of Infrastructure.” Annual Review of Anthropology 42: 327–43.
Livingston, Julie. 2012. Improvising Medicine: An African Oncology Ward in an Emerging Cancer Epidemic. Durham: Duke University Press.
Mol, Annemarie. 2002. The Body Multiple: Ontology in Medical Practice. Durham: Duke University Press.
Pantipa Sakthong and Vijj Kasemsup. 2011. Health-related Quality of Life in Thai Peritoneal Dialysis Patients. Asian Biomedicine 5, no. 6: 799-805.
Seo, Bo Kyeong. 2016. Patient Waiting: Care as a Gift and Debt in the Thai Healthcare system. Journal of Royal Anthropological Institute 22: 279-295.
Sripen Tantivess, Pitsaphun Werayingyong, Piyatida Chuengsaman, and Yot Teerawattananon. 2013. Universal Coverage of Renal Dialysis in Thailand: Promise, Progress, and Prospects. BMJ 346.
Street, Alice. 2014a. Biomedicine in an Unstable Place: Infrastructure and Personhood in a Papua New Guinean Hospital. Durham: Duke University Press.
Street, Alice. 2014b. Rethinking Infrastructures for Global Health: A View from West Africa and Papua New Guinea. Somatosphere.
von Schnitzler, Antina. 2013. “Traveling Technologies: Infrastructure, Ethical Regimes, and the Materiality of Politics in South Africa.” Cultural Anthropology 28, no. 4: 670–93.
Viroj Tangcharoensathien, Siriwan Pitayarangsarit, Walaiporn Patcharanarumol, Phusit Prakongsai, Hathaichanok Sumalee, Jiraboon Tosanguan, and Anne Mills. 2013. Health Research Policy and Systems.11, no. 25:1-9.
Wall Street Journal. June 18 2015. South Korea MERS Outbreak Brings Focus on Samsung Hospital.