In August 2016, during a science-meets-policy summit in Kampala’s famous Serena Hotel, a presentation on the (in-)effectiveness of so-called long-lasting insecticide-treated nets against malaria sparked a heated debate. The presentation was given by an infectious disease specialist from Makerere University and provided evidence that six months after the distribution of free-of-charge bed nets, only 50% of the studied households were actually using this preventive technology. To calm the discussion down, one of Uganda’s leading malariologists offered the following statement:
“Don’t go away with the impression that the nets are useless. Instead, we need to find out what caused their modest effectiveness. You know it is not like the spraying [indoor residual spraying], where it doesn’t matter how one behaves … this [the chemical] is just there! But still, we have to find out what makes the nets disappear after only 6 months …”
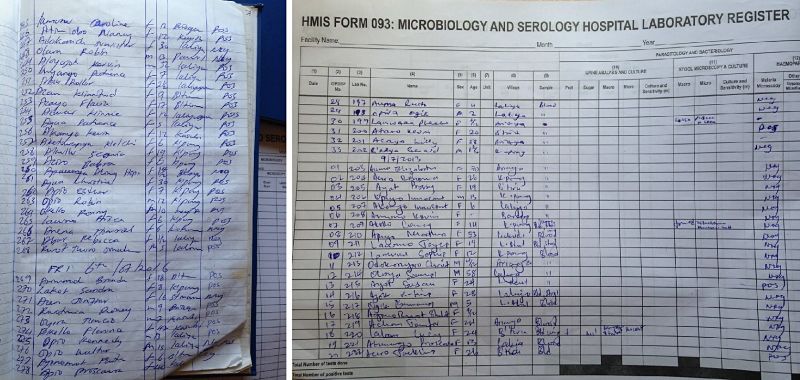
In the course of the meeting, other participants made their concerns about the study results even more explicit by indicating that donors and policy makers would not be amused to hear about them. One of the main reasons for their worries was that the Global Fund and other donors had just approved the funding of another 25 million bed nets for a second universal coverage campaign. However, a more implicit unease might have been caused by the fact that the study had been carried out in some of the country’s northern districts, which were and are directly affected by an unprecedented malaria epidemic. Since May 2015, the number of people seeking treatment for malaria has remained steadily and exceptionally high,[1] leading to severe stock-outs of antimalarial medications, diagnostic tests and blood reserves in most public health facilities.[2] Apart from mass drug administration and the deployment of some 300 additional health workers, mainly in remote facilities, the core focus of the government’s emergency interventions was on behavioral change campaigns (BCC), which were expected to help address the problem of low or inappropriate utilization of bed nets (MoH/NMCP 2015b).
The above-cited statement of the malariologist at the summit meeting directs our attention to some fundamental differences between indoor residual spraying and the distribution of insecticide-treated bed nets, two of the most prominent and strongly financed preventive technologies in current malaria control programs, and used in almost all endemic countries. While indoor spraying is implemented in a top-down manner, turning people into docile recipients of a Global Health intervention, bed nets re-configure individuals into responsibilized users. What the above statement is silent about, however, is whether and how the deployment of one technology (bed nets) can substitute for another (indoor spraying)?
Given the different ‘nature’ of the technologies, my argument is that the grounds on which indoor spraying and bed nets could be connected to one another are also changing and are strongly affected by the actual use of both technologies.
What I term ecological grounds refer to the highly dynamic relationships between mosquitoes, parasites and humans, which not only cause infections but also provide for people’s (partial) immunity against malaria.[3] I treat immunity here as an effect of what it means to live and work in malaria endemic settings, where constant exposure to infectious mosquito bites has long been the sole mode of protection.
In this post, I critically explore the relationship between the two technologies as one of a problem of connectability. Which conflicting demands, expectations and burdens are engendered both by locating the prevention/infection of malaria preeminently inside households and through the use of different technologies? I argue that the ecological grounds on which people are able to receive and use these technologies are also shifting and changing in unaccounted ways. I will show that whether and how the two technologies can actually be connected as part of a comprehensive malaria control scheme does not depend on people’s ‘behavior’ alone. Instead, I argue that it is a question of how to account for the less visible disconnections that take place simultaneously. This is because the aim of disconnecting humans and mosquitoes both rests on, as well as enacts, another less visible disconnection between humans and parasites. The case study is mainly situated in the northern districts of Uganda, where I conducted research as part of a recent seven-week fieldtrip.
Malaria and its Prevention in (Northern) Uganda
Malaria constitutes a major public health concern in Uganda, with some of the northern districts displaying the highest transmission rates in Africa (MoH/DIFD 2013). Given its high prevalence rates of malaria, Uganda became one of the major beneficiaries of Global Health programs on the continent, receiving most of its funding from the Global Fund to Fight AIDS, Tuberculosis & Malaria and the President’s Malaria Initiative (PMI). While the Global Fund in general mainly finances bed nets, diagnostic tools and antimalarial drugs, the largest share of the annual budget for USAID’s PMI is allocated to indoor spraying (approximately US$20 million, see USAID/PMI 2008-2015).
Beginning in 2008 with some pilot districts, the recorded impact, together with the available financial resources, led to a scaling up of indoor spraying to about 10 districts in Northern Uganda (USAID/PMI 2009). It is known from entomological experiments that mosquitoes rest on walls before or after blood meals. Coating the walls or ceilings of houses with a chemical pesticide therefore forms the central element of indoor spraying. Mosquitoes and other insects that come into contact with or close to these surfaces are either killed or repelled. According to the revised guidelines of the WHO (WHO 2007), indoor spraying involves the sprayer conducting himself in an almost Tayloristic manner, applying the insecticide to the interior walls of a house/hut while practicing meticulous bodily control and a sound choreography of the pump and nozzle.[4] To get an impression of the techniques involved, I quote from an official WHO manual:
“Apply spray in vertical swathes 75 cm wide, with an overlap of 5 cm. Spray from roof to floor, using a downward motion, to complete one swathe. Step sideways and spray upwards from floor to roof. (…) Time your spray speed to cover one meter every 2.2 seconds, i.e. 4.5 seconds for a 2 m high wall. Timing may be aided by mentally counting ‘one thousand and one – one thousand and two – one thousand and three’ (…) Adjust the mental counting procedure according to the local language (WHO 2007).”
More important for the case presented here is that prior to the spraying, the dwellings must be cleared completely of furniture, food and livestock.
The massive mobilization and coordination of people, equipment, furniture and livestock often results in tense encounters between spraying teams and communities.
In some districts, it was frequently reported that people were threatened or harassed if they refused to get their homes sprayed (ABT/PMI 2011). A central condition for sustaining the efficacy of indoor spraying is that at least 80% of the habitations of a specified terrain need to be sprayed. Thus in cases where this is not achieved, the hired companies will face pressure from or even the dissolution of contracts with USAID. For all involved parties, it is clear that indoor spraying in its top-down manner constitutes a harsh intervention. Carried out at least twice annually or every six months, indoor spraying invokes the image of an intrusive bio-political tool of archaic provenance. However, on the representational (political) level it can easily be translated into ‘protected populations’ (PMI/USAID 2014). The logic behind ‘protected populations’ that are ‘shielded indoors’ rests on a notion of a holistic intervention with almost hermetical qualities, disconnecting both humans from mosquitoes, as well as environments from the toxicities of chemicals.
Given the complex relationship between the various environments and different species involved, it has been suggested that malaria is best conceived of as a disease or something that circulates between humans, mosquitoes and parasites (Turnbull 1989, Kelly & Beisel 2011). One effect of this complex interspecies interaction is that people develop some degree of ‘naturally’ acquired immunity (Langhorne et al. 2008). A crucial driver of this immunity is the yearlong and constant exposure of people to infectious mosquito bites (estimation of at least five infective bites per person per year, Doolan et al. 2009). While immunity does bear some relationship to non-adherence and the risk of drug resistance (Umlauf 2015) – i.e. because weak symptoms in adults tend to disappear after taking half a dosage of antimalarial medications, although no full clearance of parasites has occurred – more importantly, it is also assumed that immunity has provided the foundations for populations’ survival/co-existence with mosquitoes and malarial parasites for many centuries, since long before colonialism.
My emphasis on the role that immunity might have played in human survival in endemic regions should not, however, downplay the precariousness, suffering and risks inscribed in acquiring malaria.
This is particularly the case for children under five, who are not only the most vulnerable but need to be steered trough life-threatening episodes of the disease.
Locating the Epidemic
Without having any reliable scientific evidence (to date), the current national crisis narrative in Uganda pinpoints the onset of the epidemic outbreak of malaria in the ten northern districts to more or less six months after the last spraying episode was carried out in October 2014. No further sprayings had been planned thereafter. The anecdotal evidence I was able to collect from USAID as well as from Ministry of Health officials legitimated this termination of indoor spraying, both in relation to the significant decline in prevalence rates as well as the roll-out of the universal bed net campaign. Between August 2013 and October 2014, over 22 million bed nets were distributed throughout the entire country (GoU 2014). On the basis of the low prevalence rates for malaria cited in health statistics, it was concluded that bed nets could now substitute for the costly spraying as a more cost-effective intervention that would ultimately help to sustain the public health gains (USAID/PMI 2015).
At that very moment, nobody was aware or wanted to acknowledge that this assessment was based on a gross underestimation of the grounds on which these ‘gains’ had been achieved through people’s immunity.[5]
Before I turn to the mutations and transformations in the role of bed nets following the suggested disconnection of humans and parasites, I want to briefly outline the relationship between preventive technologies and mosquitoes. I suggest that there is an often little considered side effect of this relationship that is related to the adaptive capacities of Anopheles gambiae, the most prevalent vector of malaria in Northern Uganda (personal conversation with entomologist in Gulu). Locating and concentrating almost all efforts in domestic spaces exercised considerable pressure on the mosquitoes’ behavior, as well as on their biology (Russel et al. 2011). While it is likely that the number of mosquitoes are reduced on treated interior walls, it has also been observed that this pressure triggers resistance to the applied pesticides. In addition to acquiring resistance, mosquitoes also adapt their biting behavior and change both their preferred time and place of feeding, resulting in new and unexpected configurations of where and when infections take place (Beisel 2015).
Bed Nets: An Option with no Choice…
Given the preeminently private nature of the everyday use of bed nets, only a few (ethnographic) studies have so far been carried out on the issue (Winch 1999, Panter-Brick et al. 2006). While bed nets are commonly claimed to be a simple and highly effective solution within Global Health circuits, people more often than not tend to treat them as an option but not a necessity. A popular and often raised concern against more frequent use is the discomfort people experience when sleeping under a net. In such cases, bed nets are perceived to further reduce air-circulation in already humid and sticky places (Wanzira et al. 2014). On a more technical or practical level, the fragile materiality of bed nets regularly renders them a rather inappropriate technology. It seems that the script of the nets anticipates more ‘modern’ living conditions, where there is a stronger division between sleeping and living areas than is realistic in many African settings. Many rural households are not divided along these lines and lack a designated sleeping room. Consequently, mattresses and other sleeping equipment need to be (re)moved on a daily basis to transform the bedroom into a daytime living space. The embroiling of bed nets into these activities adds another layer of laborious tasks and also increases the risk of tears, thus rendering the technology nearly ineffective. In addition, mosquitoes can develop resistance to the bed net insecticide (N’Guessan et al. 2007). While this latter issue has not actually been reported for Northern Uganda, it was the relative lack of mosquitoes – and the reduction of the nuisance – that made people perceive the nets as an impractical and unnecessary option.[6]
As was indicated in the quote cited at the beginning of this post, the difference between indoor spraying and bed nets is that the effectiveness of the latter depends on people’s behavior and living conditions.
Bed nets shift responsibility, from a person being a passive recipient to becoming a subject whose behavior has to be changed and who cares about the use and utility of the technology. In light of the described potential interference with people’s immunity through the continuous use of indoor spraying, however, I argue that the epidemic crisis reveals a more fundamental transformation, whereby an ‘impractical’ technology is silently turned into the only viable option to prevent malaria. The main problem in this regard is that most people are unaware of this transformation, particularly because they are unaware of their disconnection from their own immunity. Although at the height of the epidemic people were constantly complaining to nurses that this malaria was more severe or of a different origin than former episodes, most of them were not aware of the connection between indoor spraying and their reduction in acquired immunity. When I asked the District Health Officer of Gulu District if it would have been better to make the conflicting relationship between indoor spraying and people’s immunity part of risk communication, he laughed nervously and explained:
“You see, that would be even more complicated. The situation is similar to HIV; we don’t tell the people that it is actually pretty hard to contract the virus… instead we tell them a single unprotected contact is enough…”
The subtext to the statement is that publicly announcing a connection between indoor spraying and people’s reduced immunity (e.g. as part of a behavior change campaign for bed nets) would potentially increase the reservations that people already had to getting their homes sprayed twice a year. In turn, refraining from including this information in behavior change campaigns excludes a vital point for communicating the utilization of bed nets as a necessity with existential implications.
It is clear that the changing ecological grounds on which the transformation of bed nets is taking shape – from an impractical option to an option without choice – are not being openly communicated, and given the accompanying complexities most likely never will be.
The mentioned impracticalities of bed net utilization, together with the non-communicated side effects of indoor spraying, contribute to a dislocation of the origins of the malaria epidemic. The epidemic is now treated as a problem of behavior change rather than a problem of changing ecological grounds.
Disconnecting humans from mosquitoes within households through the use of indoor spraying is likely to have affected another vital connection between humans and parasites. The current focus on ‘behavior’ and ‘behavior change’ instantiates a prominent framing of the (side) effects that Global Health technologies produce for and within the intervention contexts. In the presented case, behavior change refers to the expectations that public health experts have of how people should determine or negotiate the utility of bed nets in light of changes in both mosquitoes’ behavior as well as in immunity levels. However, as I have shown, behavior can neither account for the demonstrated impracticalities nor for the fact that infections are occurring outside of bed nets and posing an increased risk of suffering more severe and potentially life threatening episodes of malaria. We could equally say that the changes in the relationship between mosquitoes, parasites and humans have rendered bed nets an even more impractical option, with no other choice for many people than to face new precarious levels of exposure in order to acquire fresh immunity.
Co-published by Allegra Lab and the Collaborative Blog Medizinethnologie: Body, Health and Healing in an Interconnected World
References
ABT/PMI. 2011. “Uganda Indoor Residual Spraying (IRS) Project Annual Performance Report, October 1, 2010 through September 30, 2011.” United States Agency for International Development Kampala, Uganda. .
Beisel, Uli. 2015. “Markets and Mutations: Mosquito Nets and the Politics of Disentanglement in Global Health.” Geoforum 66 (November): 146–55.
De Zulueta, J., G. W. Kafuko, J. E. Cullen, and C. K Pedersen. 1961. “The results of the first year of a malaria eradication pilot project in northern Kigezi (Uganda).” East African Medical Journal 38 (1): 1–26.
Doolan, Denise L., Carlota Dobaño, and J. Kevin Baird. 2009. “Acquired Immunity to Malaria.” Clinical Microbiology Reviews 22 (1): 13–36.
Government of Uganda (GoU). 2014. “Universal Coverage of LLINs in Uganda – Insights into the Campaign Implementation.” Kampala, Uganda: Government of Uganda and Stop Malaria Project (USAID).
Kelly, Ann H., and Uli Beisel. 2011. “Neglected Malarias: The Frontlines and Back Alleys of Global Health.” BioSocieties 6 (1): 71–87.
Langhorne, Jean, Francis M. Ndungu, Anne-Marit Sponaas, and Kevin Marsh. 2008. “Immunity to Malaria: More Questions than Answers.” Nature Immunology 9 (7): 725–32.
MoH/DFID. 2013. “An Epidemiological Profile of Malaria and Its Control in Uganda. A Report Prepared for the Ministry of Health, the Roll Back Malaria Partnership and the Department for International Development, UK.” Kampala, Uganda: National Malaria Control Program, Ministry of Health.
MoH/NMCP. 2015a. “Uganda Malaria Quarterly Bulletin Issue 9: January — March 2015.” Ministry of Health, Kampala, Uganda.
———. 2015b. “Uganda Malaria Quarterly Bulletin Issue 11: July — Sept 2015.” Ministry of Health, Kampala, Uganda.
———. 2016. “Malaria Bulletin – National Malaria Control Program Issue 1, Volume 1, January – April 2016.” Ministry of Health, Kampala, Uganda.
Molineaux, Louis, and Giovanni Gramiccia. 1980. “The Garki Project. Research on the Epidemiology and Control of Malaria in the Sudan Savanna of West Africa.” Geneva: World Health Organization (WHO).
N’Guessan, Raphael, Vincent Corbel, Martin Akogbéto, and Mark Rowland. 2007. “Reduced Efficacy of Insecticide-Treated Nets and Indoor Residual Spraying for Malaria Control in Pyrethroid Resistance Area, Benin.” Emerging Infectious Diseases 13 (2): 199–206. doi:10.3201/eid1302.060631.
Panter-Brick, Catherine, Sian E. Clarke, Heather Lomas, Margaret Pinder, and Steve W. Lindsay. 2006. “Culturally Compelling Strategies for Behaviour Change: A Social Ecology Model and Case Study in Malaria Prevention.” Social Science & Medicine, 62 (11): 2810–25.
Russell, Tanya L., Nicodem J. Govella, Salum Azizi, Christopher J. Drakeley, S. Patrick Kachur, and Gerry F. Killeen. 2011. “Increased Proportions of Outdoor Feeding among Residual Malaria Vector Populations Following Increased Use of Insecticide-Treated Nets in Rural Tanzania.” Malaria Journal 10 (April): 80.
Stengers, Isabelle. 2005. “Introductory Notes on an Ecology of Practices.” Cultural Studies Review 11 (1): 183–96.
Turnbull, David. 1989. “The Push for a Malaria Vaccine.” Social Studies of Science 19 (2): 283–300.
Umlauf, René. 2015. “Mobile Tests – Einfaches Wissen. Zur Laboratorisierung und Projektifizierung der Malariadiagnose im ländlichen Uganda.” Unpublished PhD Thesis, University of Bayreuth.
USAID/PMI. 2008. “Uganda – Malaria Operational Plan FY 2008-2015.” United States Agency for International Development Kampala, Uganda.
Wanzira, Humphrey, Adoke Yeka, Ruth Kigozi, Denis Rubahika, Sussann Nasr, Asadu Sserwanga, Moses Kamya, Scott Filler, Grant Dorsey, and Laura Steinhardt. 2014. “Long-Lasting Insecticide-Treated Bed Net Ownership and Use among Children under Five Years of Age Following a Targeted Distribution in Central Uganda.” Malaria Journal 13: 185.
WHO. 2007. “Manual for Indoor Residual Spraying: Application of Residual Sprays for Vector Control.” World Health Organization, Geneva.
WHO/NMCP. 2015. “WHO’s Assessment of Malaria Epidemics in Uganda. Findings and Recommendations.” Kampala, Uganda: Unpublished document.
Winch, Peter J. 1999. “The Role of Anthropological Methods in a Community-Based Mosquito Net Intervention in Bagamoyo District, Tanzania.” In Anthropology in Public Health: Bridging Differences in Culture and Society, edited by Robert A. Hahn, Oxford University Press, Oxford, England ; New York, 44–62.
[1] The number of diagnosed malaria cases (lab confirmed and clinical) per month rapidly doubled in the quarter from April to June 2015, from the lowest (829,548 cases) recorded in over two years to the highest (1,629,237) since July 2013 (MoH/NMCP 2015a). While the numbers represent cases throughout the entire country (111 districts), the rise in numbers took place predominantly in the 10 epidemic districts. Between May and September 2015, Gulu district, for instance, registered over 140,000 cases in their public health facilities, indicating a tenfold increase compared to the years before (see also http://www.newvision.co.ug/new_vision/news/1409038/gulu-start-mass-anti-malaria-treatment).
[2] One of the crisis meeting reports put together by a national task force team stated: “It is likely that the poor district data is masking (under-estimating) the magnitude of the epidemic in the affected districts. From the field observations and interviews, it can be concluded that the national response is too little and too late to cope with the magnitude of the current epidemic which is affecting large segments of the population in such a short time” (WHO/NMCP 2015).
[3] For the use and understanding of the conceptual underpinnings of ecology in this paper, see Isabelle Stengers ‘Introductory Notes on an Ecology of Practices’ (Stengers 2005).
[4] In older versions, ‘indoor’ also included so-called ‘ingress surfaces’, i.e. those surfaces on the exterior of dwellings that the mosquito might come into contact with when gaining access to the interior (DeZuleta et al. 1961). However, increased environmental concerns over pesticides migrating to the outside led to the adaptation of the new version.
[5] Ceasing indoor spraying without any sustainable ‘exit strategy’ in place also hints to a degree of collective oblivion in Global Health interventions with regard to its own history. What has been called the ‘Garki Project’ was one of the largest and best documented epidemiological experiments on the African continent regarding the use of indoor residual spraying, and provides (historical) evidence for how long-term spraying (between 1969-75) affects parasitemia levels and thus people’s immunity (Molinaux & Gramiccia 1980).
[6] See also http://www.mghcgh.org/stories-from-the-field/studying-the-barriers-to-antimalarial-bednet-use-in-uganda/.



This is an insightful article! And very informative as well. As a BCC practitioner, I better understand the enormity of communicating Malaria-related ‘behaviour change’
Did you get permission from these patients to share their test results online? If not, this image is a breach of patient confidentiality.