Medical genetics has long gone global. From WHO recommendations and travelling bioethics experts and DNA samples, to disease-related Facebook groups and national genome projects, its circulation routes and shades of glocalization are numerous. Among these manifold forms of connectivity, the following – deceptively anecdotal – example is telling: the US actress Angelina Jolie, as a carrier of a pathogenic mutation of the BRCA1 gene, decided to undergo risk-reducing surgery, publically announcing it in 2013 (Jolie 2013). The news swiftly spread throughout the world and doctors soon coined the phrase ‘Angelina Jolie effect’ to describe the sharp increase in BRCA screening requests that they observed (Evans et al. 2014).
This transnational effect of an individual medical choice has been observed in genetics clinics worldwide, showing once again how hyper-connectivity and globalization impact individual health decisions.
However, the presence and actual manifestation of a genetic disease are also components of a ‘local biology’ (Lock and Nguyen 2010) shaped by numerous factors, including environment, marriage patterns, as well as health policies and infrastructures (e.g. about cancer in Botswana, see Livingston, 2012). The social meaning of genetic knowledge is framed by dimensions such as local understandings of consanguinity (Beaudevin 2015), ‘colonial histories of migration, the embodied effects of dietary habits, or [even] the moral failings of near and distant ancestors’, as shown by Sahra Gibbon (2013) in Brazil.
In this contribution, I trace the shifts in medical genetics as it circulates within, to and from the Arabian Peninsula, more specifically the Sultanate of Oman. In doing so, I draw on my previous fieldwork in Oman looking at obstetrical ultrasound and haemoglobinopathies, as well as on my ongoing anthropological research focused on medical genetics, genomics and public health in the Sultanate. I recently began to conduct ethnographic research at the country’s two genetic medicine centres, observing everyday clinical work and interviewing patients, families and staff. I aim to explore a field that is attempting to thrive despite the high costs induced by training specialists and paying for the machines.
Documenting the manifestations of medical genetics in Oman therefore means exploring the manifold ways of caring, diagnosing, treating, coping with and understanding genetic disorders, while navigating a highly specialized scientific and medical field, and an ongoing process of resource limitation.
I intend to use the opportunity of this publication to embark on an exploration of my current work with an approach I have not used so far: I will examine several recent examples from my fieldwork as part of a ‘landscape of rarity’, through the combined lenses of exceptionality [1] and scarcity. I aim to shed light on the importance of adaptation and tinkering practices in the everyday work of medical genetics. I also emphasize the ways in which genetics circulates to, in and from Oman, and explore some of the connections and mobilities that appear when exceptionality or scarcity characterize tools, people, funds or knowledge in the field of medical genetics.
Of Oil and Health
In the Sultanate of Oman, genetic medicine has been part of the healthcare system for many years. It partly began with the diagnosis and community genetics management of haemoglobinopathies, especially sickle-cell anaemia and beta-thalassaemia. This pattern is shared with other countries (Modell and Kuliev 1998 and Modell, 2016, interview) and is unsurprising given both the relative affordability and technical ease of diagnosis conducted on haemoglobin itself (i.e. genetic analysis per se is not required) and the high incidence of haemoglobinopathies in the region. In recent years, under the umbrellas of the Ministry of Health and the Sultan Qaboos University Hospital, two public genetic medicine centres have been created in Muscat, the Omani capital, each providing an on-site combination of genetic expertise, diagnostic facilities and genetic counselling.
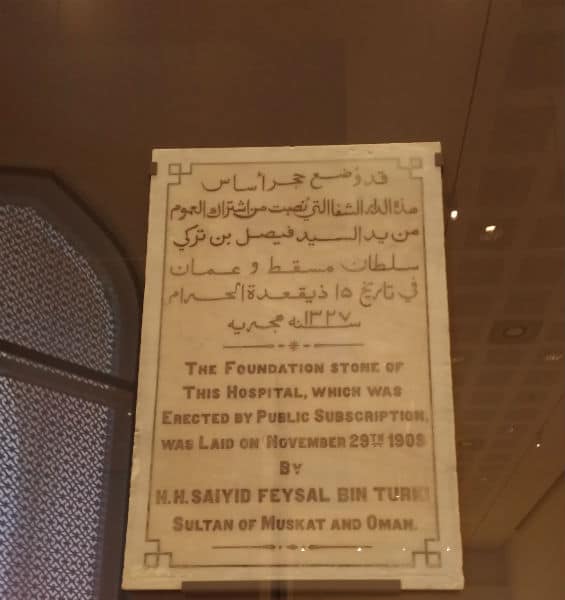
These two centres operate in the context of an authoritarian monarchy with a population of 3.5 million inhabitants, which has seen extensive economic and social changes since the current Sultan’s accession to the throne in 1970. At that time, the country was deprived of almost all infrastructure. This scarcity applied to healthcare as well: a small American missionary hospital located in Muscat was the country’s sole biomedical health facility (see picture 2).
The oil-financed modernization plan that was launched in the 1970s, which addressed administration, health, education, industry, etc., transformed Oman into a relatively wealthy country that enjoys a somewhat unusual degree of stability in the region.
In contemporary Oman, most public funds still originate in oil rent, and therefore constitute shared benefits from oil extraction rather than the shared redistribution of taxes paid by citizens.
Regarding the scientific scene, Oman’s remoteness from the main historical scientific centres of the former Arab and Ottoman empires led to a sparse landscape of local research institutions. This situation persists today, despite the creation of the Sultan Qaboos University in the capital in the 1980s. In this specific social and political context, and following the implementation of an efficient countrywide primary healthcare network, the government is currently facing new challenges, especially related to chronic and non-communicable disorders. Among them, genetic diseases are considered a major public health problem and are thus being targeted by new policies.
Reading Medical Genetics through Rarity
When writing this contribution, and still under the impression of my recent fieldwork, I struggled to make sense of the richness of the encounters I had. I eventually realized that while researching medical genetics and analysing my fieldwork data, again and again I have found myself roaming in the semantic and conceptual field of rarity. More specifically, I see manifestations of both of rarity’s dimensions, namely exceptionality and scarcity.
I met people affected by rare disorders due to uncommon genetic mutations. These disorders are diagnosed and investigated by the handful of trained specialists working in the country in the two dedicated centres.
The options offered to patients or to couples at risk of having an affected child are limited by factors including the rareness of institutions designed to help individuals with disabilities, the growing but still limited number of local testing and prenatal diagnosis facilities (see about this: Bruwer et al. 2014, Bruwer, Al-Foori, and Al-Kharousi 2014), and the absence of pre-implantation genetic diagnosis in the country.
On a macro scale, the backdrop to the current expansion of medical genetics in Oman also involves limitations: the aftermath of the 2008 global financial crisis, combined with the current drop in oil prices, has led the Omani government into unfamiliar territory. Deficits usually absorbed by state finances were in 2016 managed for the first time partly through massive public budget cuts and shortages (Valeri forthcoming, 2017, Reuters 2016, Oman News Agency 2015, 2016). This has begun to affect health-related expenditures in the public sector. This situation is not unique to Oman, however: cuts in resources allocated to health (related to financial crises and structural adjustments) are having major impacts on healthcare systems and individual health decision-making worldwide, the most recent European examples being Greece and Spain (Brand et al. 2013, Karanikolos et al. 2013, Kehr 2014, Pfeiffer and Chapman 2010).
When Rarity Begets Value and Suffering
Medical genetics in the Gulf encompasses a dialectic of abundance and singularity: the field targets both a myriad of rare disorders and more common inherited conditions, whose aggregate constitutes a massive clinical field. This ensemble is considered a relevant target for public health, which justified the creation of the two genetic medicine centres. Another dialectic deals with the impact of specific genetic profiles, and articulates value and suffering. Partly because of the widespread practice of consanguineous marriage (about 25-35 per cent of married couples in the region are first cousins, and Oman is no exception), the genetic profile of Gulf populations is quite specific.
This exceptionality shapes the composite ontology of the gene pool: on the one hand, it is a desirable object of scientific enquiry; on the other, it is a heavy burden for patients, families and healthcare systems that must face poorly investigated disorders or conditions with no available treatment (for anthropological work about consanguinity in Oman, see Beaudevin 2015; in Qatar, see Kilshaw, Al Raisi, and Alshaban 2015).
Scientific desirability shapes multiple mobilities, primarily of researchers and DNA samples that travel between Oman and various international research institutions in Europe and North America. Many affected individuals are aware of this entanglement of scientific value and their own experience. One Omani man I met, whose family is affected by a severe, lethal and incurable neurological disorder, for instance, told me about a foreign clinician’s ‘excitement’ upon realizing that about 20 members of his family showed symptoms (interview, Muscat, 2016). Nonetheless, this man has also made use of the intense connectivity characterizing such research: he was the one who originally looked up the clinician online on the basis of his research interests.
Scientific events where clinicians and scientists gather illuminate the dialectical pairs mentioned above: first, the presentations tackle manifold disorders that sometimes impact only a very small number of families; second, the papers deal both with the daily issues faced by affected individuals and with the pride of describing new syndromes and mapping new genes. A biennial gathering of genetics experts from the Arab world (with guest speakers from Europe and North America), the Pan-Arab Human Genetics Conference held in Dubai, offers an example of such an event.

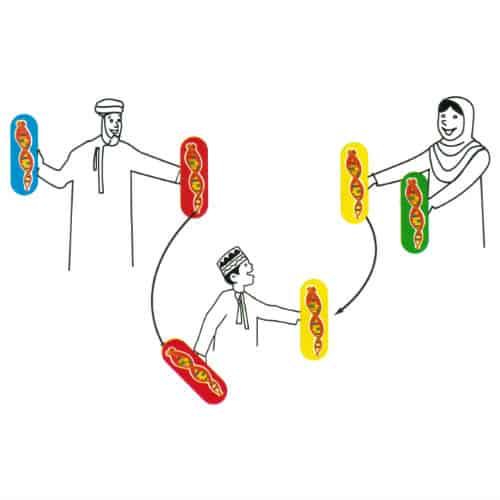
During its 6th edition organized in January 2016, a keynote speaker candidly asserted that consanguinity is both ‘an important problem and an opportunity to identify pathogenic variants’ (Antonarakis 2016). Another speaker concluded in a more subtle way that ‘investment in genomics in this part of the world [the Middle East] will be highly valuable’ (McCarthy 2016). Slides and posters display the emblematic visual representations that encompass the ambiguous status of medical genetics research. The ‘family pedigree’, for instance, a biomedical species of family tree, is a scientific tool that helps materialize the singularity of an individual’s/family’s genetic profile. Picture 3 shows such a ‘research pedigree’, taken from a scientific poster presented in an earlier edition of the Pan-Arab Human Genetics Conference (Al-Mejni et al. 2007).
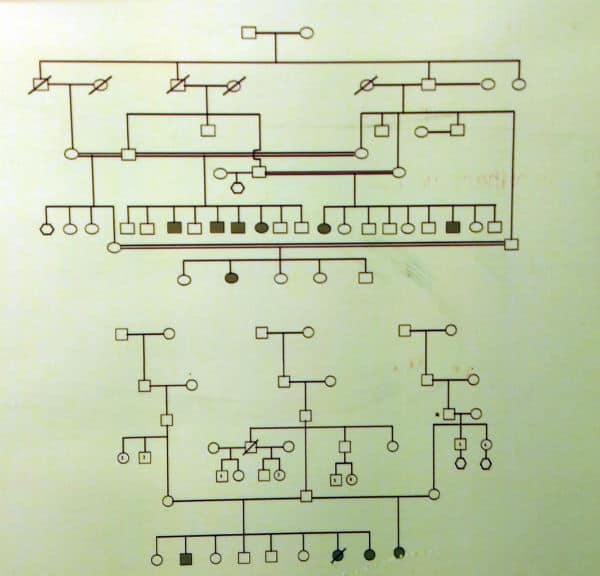
Circles represent female family members, squares represent males, hexagons show individuals of unknown gender; they are struck through if the individual is deceased and coloured when s/he is affected by the studied condition. Marriages are noted with horizontal lines, descent by vertical lines. The original caption of picture 4 read ‘Informative pedigrees showing the complexity of family structure’. This complexity matters because it is implicitly defined in contrast to ‘Western’ family patterns. It includes: number of children (up to nine here), successive first cousin marriages (double horizontal lines), and polygamy (a square linked by horizontal lines to two different circles, none of them struck through, i.e. all individuals are alive). Picture 5 below shows an example of the ‘clinical pedigree’ that is drawn in front of a patient by a clinician or a genetic counsellor, who asks numerous questions about the patient’s family history and structure in order to fill it out.
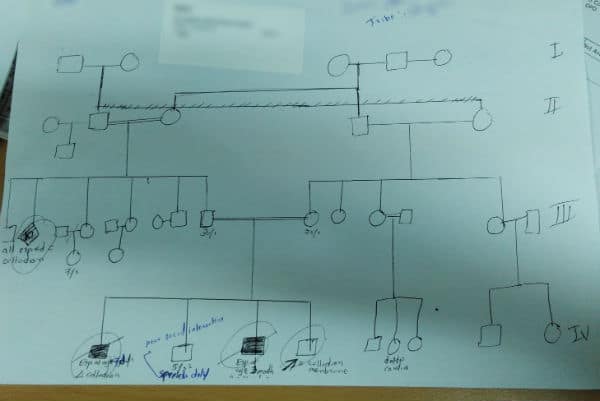
This example displays consanguineous marriage and polygamy and bears traces of the conversation between the patient and the medical genetics professional: corrections, ages, causes of death, clinical information about a child’s development, etc. This handwritten version bears more evidence of the family’s suffering than the research pedigree showed above. Just like DNA samples themselves, these peculiar pedigrees embody the value of the Omani gene pool for genetic research purposes: picture 5 displays four generations and shows families of four to six children, two consanguinity links and a probably polygamous great-grandfather, as well as several affected family members — including the one who came to the consultation, pointed at by an arrow.
When Exceptionality Leads to ‘Infrastructural Disconnectivity’ and Necessary Mobilities
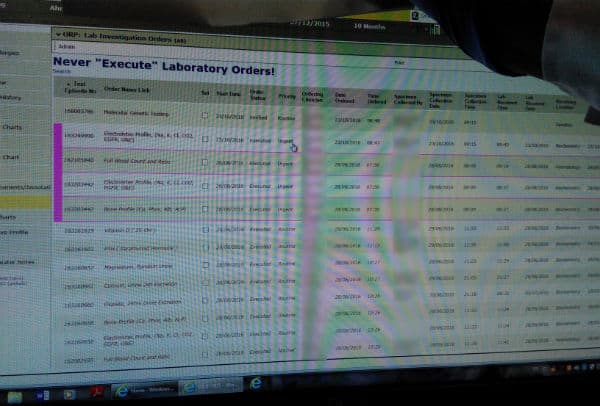
In Oman as elsewhere, medical hierarchy impacts therapeutic itineraries. The novelty of the profession of genetic counselling in the country and the very small number of formally trained practitioners deprive this activity of a clear status in the medical hierarchy. Genetic counsellors are mostly locally trained as nurses or biologists before travelling abroad for specialization in countries where genetic counselling is an established activity. They study in places such as the UK, USA and South Africa, depending on their personal networks as well as Oman’s historical connections. In their everyday practice of counselling, they are sometimes limited to the ‘box’ of their original education. For example, the various software used for managing patient information (picture 6 shows one such interface) allow data access and entry on the basis of professional status. Nurses may thus not be ‘allowed’ to request further tests — or rather, they may be technically prevented from doing so — just as biologists may not be granted access to add remarks in the ‘medical’ fields of a patient file, even if their genetics-related activities require them to do so. For all of the genetics counsellors, negotiating their new status in the healthcare system is directly related to fixing what one could call infrastructural disconnectivity between various parts of the system: the medical results they can access onscreen, the referrals they are allowed to arrange, and the field dedicated to their remarks in the patient file are all crucial matters for them to control, since they determine the smoothness of a patient’s therapeutic itinerary.
There are also other kinds of infrastructural disconnectivities at play. One can almost count the number of trained clinical geneticists and genetic counsellors working in the country on two hands. This creates a strong centralization of expertise in the capital area, in the two centres already mentioned, which are considered tertiary healthcare facilities. In an attempt to spread expertise outside of the capital, an 18-month training program in genetic counselling was initiated in 2014 at the National Genetic Centre, and has been attended by nurses from different governorates. Nevertheless, the current state of centralization begets numerous necessary mobilities: most patients and families searching for a diagnosis or expecting test results have to travel from all over the Sultanate to attend the clinics in the capital. For those affected by disorders requiring follow-up, these travels become part of a routine (Beaudevin 2013a, b).
Travelling abroad for tests or treatment is also very common, in order to seek a second opinion or a treatment that is locally unavailable.
In the latter case, these mobilities are partially institutionalized: there exists a regulatory framework that involves a ‘recommendation for treatment overseas’, which can be filed by a specialized doctor following the patient. For Omani nationals, such a referral can lead to the cost of travel and treatment being covered by public funds.
Of Financial Scarcity Management
The current development of the medical genetics field follows a path marked out by the WHO: the organization, through its dedicated programs (Hereditary Diseases until 1995, Human Genetics until 2016, and now Human Genomics and Public Health), has repeatedly advocated for community genetics interventions aimed at organizing testing and genetic counselling for common hereditary disorders: first in the world’s wealthiest countries in the 1980s, then in ‘developing’ countries in the 1990s (World Health Organization 1999). As diagnostic tools became more affordable, the WHO recommended in 2010 that preventing congenital disorders within primary healthcare would imply developing ‘pre-conception care, population screening, genetic counselling, and the availability of diagnostic services’ (World Health Organization 2010). Against this backdrop, and facing both epidemiological transition and notable rates of consanguinity, in the last decade Oman and other Gulf countries have started to implement relevant policies.
The context and possibility of such decisions, however, changed very recently. The current drop in oil prices had a strong impact on the economies of countries considered solidly wealthy — Saudi Arabia is archetypal of this; for Oman, see for instance Oman News Agency (2016). Economic uncertainty is admittedly not unknown in Oman and many Omanis have long been concerned about the future. Nonetheless, as mentioned above, it was only as recently as 2016 that they saw the first occurrence of official public funding cuts.
Readers may wonder how dropping oil prices are relevant to a medical anthropologist researching genetics.
Aside from the general impact on healthcare systems, part of the answer actually lies in the encounter between shortage and newly-introduced biomedical technologies that involve heavy investments (for machines, as well as in training) and high functioning costs. Some interventions – chiefly the tests necessary for pre-implantation genetic diagnosis performed abroad – are, since the beginning of 2016, no longer government funded. This change in funding will probably not stop the flow of patients travelling for genetic testing purposes, but it will definitely increase inequalities in access, adding money to the list of requirements that determine a person’s ability to travel.
The combination of specific requests from clinicians and the economic situation creates necessities for trade-offs in medical genetics and genomics laboratories: about implementing a specific test onsite or rather requesting it from foreign companies; about selecting these companies; about the frequency at which one runs a machine (and thus uses consumables); etc. The intense connectivity of the global medical genetics milieu plays a major role in these arbitrations: the availability of reliable companies able to perform specific tests or the choice criteria used for buying a sequencing machine, for instance, are matters discussed over international networks of shared expertise.
Conclusion
Exploring medical genetics in Oman through rarity allows for an emphasis on the local biological, social and political specificities that shape both medical genetics as a research field as well as genomes per se. The Omani tribal system, part of what Fredrik Barth (1983) called the Omani ‘social diversity system’, is an organizing force in the Omani rare gene pool, since the maintenance of this system requires endogamy, and even consanguinity. Furthermore, this approach leaves space for an emphasis on the creativity of professionals and patients who must navigate a shifting field with flexibility. In addition, exceptionality and scarcity represent much more than the two sides of the rarity coin: they are closely entangled in the everyday impact of the small number of trained professionals in the country, as well as in the often ‘guilty fascination’ characterizing many foreign scientists’ approach to Arabian DNA. Rarity, in all of its shades, triggers intense connections between researchers, between Omani patients and foreign clinicians, etc. It also fuels the transnational mobility of DNA, patients, experts and technologies.
Finally, this note is but preliminary and much remains to be explored in terms of medical genetics as it is practiced in Oman, especially in clinical activities. In fact, even if the discipline of bioethics is being spread as a global framework and has been described by numerous social scientists as ‘unaware of its own socio-cultural context’ (Rapp 2000, 44), its implementation in everyday medical practices is shaped by local moral worlds. The exploration of this, including the fragmentary regulatory frameworks prevalent in genetics and the resulting impact on clinical situations, is therefore crucial.
Funding and ethical clearances
This research is funded through the Globhealth project (European Research Council) and the French National Centre for Scientific Research, and was approved in Oman by the Medical Ethics and Scientific Research Committee of the Royal Hospital and the Medical Research Ethics Committee of Sultan Qaboos University Hospital.
Acknowledgments
My gratitude goes to the professionals, patients and families who agreed to share their insights with me and allowed me into their consultation rooms, offices, labs and homes. My thanks also go to the editors for their invitation and comments, to Andrew McDowell, Ashveen Peerbaye and Caroline Meier zu Biesen for their careful reading, to Marc Valeri and Janina Kehr for their bibliographical hints and to Zoe Goldstein for her proofreading.
Co-published by Allegra Lab and the Collaborative Blog Medizinethnologie: Body, Health and Healing in an Interconnected World
References
Al-Mejni, R., A. Al-Maawali, KJ Dick, Anna Rajab, Abeer Al-Sayegh, Aisha Al-Shehi, W. Bashir, A. Al-Moundary, RI Koul, AH Crosby, and Sandy Raeburn. 2007. “FamGUARD: paving a way for molecular services in Oman [poster].” 2nd Pan-Arab Human Genetics Conference, Dubai, 20-22/11/2007.
Antonarakis, Stylianos. 2016. “From Genome Exploration to the Genome Clinic (keynote lecture).” 6th Pan-Arab Human Genetics Conference, Dubai, 20-23/01/2016.
Barth, Fredrik. 1983. Sohar: culture and society in an Omani town. Baltimore (Mass.) ; London: Johns Hopkins University Press.
Beaudevin, Claire. 2013a. “Of red cells, translocality and origins: inherited blood disorders in Oman.” In Regionalizing Oman. Political, economic and social dynamics, edited by Steffen Wippel, 91-105. Dordrecht, Heidelberg, New York and London: Springer Science.
Beaudevin, Claire. 2013b. “Old diseases & contemporary crisis. Inherited blood disorders in Oman.” Anthropology & Medicine 20 (2):175-189.
Beaudevin, Claire. 2015. “Cousin marriages and inherited blood disorders in the Sultanate of Oman.” In Cousin marriage: between tradition, globalisation and genetic risk, edited by Alison Shaw and Aviad E. Raz, 65-87. London and New York: Berghahn.
Brand, H, N Rosenkotter, T Clemens, and K Michelsen. 2013. “Austerity policies in Europe–bad for health.” British Medical Journal 346 (jun13 1):f3716–f3716. doi: http://doi.org/10.1136/bmj.f3716
Bruwer, Zandrè, Udayakumar Achandira, Khalsa Kharousi, and Adila Al-Kindy. 2014. “Existing Challenges Associated with Offering Prenatal Genetic Diagnosis in an Arab Society in the Sultanate of Oman.” Journal of Genetic Counseling 23 (6):928-932. doi: 10.1007/s10897-014-9764-x.
Bruwer, Zandrè, Amel Al-Foori, and Khalsa Al-Kharousi. 2014. “Exploring the Need for Prenatal Diagnosis and Termination of Pregnancy in Oman: The unspoken challenges.” 2nd Genetics Conference: Genetics in developing countries, unique challenges and opportunities, Sultan Qaboos University, Muscat, Oman, 9–11 March 2014.
Department of Inherited Blood Disorders (Ministry of Health) and Ministry of Social Affairs. n.d. Discovering genetic health. My mother and me would love to know the secrets of genetics. Muscat: Ministry of Health.
Evans, D. Gareth R., Julian Barwell, Diana M. Eccles, Amanda Collins, Louise Izatt, Chris Jacobs, Alan Donaldson, Angela F. Brady, Andrew Cuthbert, Rachel Harrison, Sue Thomas, Anthony Howell, Zosia Miedzybrodzka, and Alex Murray. 2014. “The Angelina Jolie effect: how high celebrity profile can have a major impact on provision of cancer related services.” Breast Cancer Research 16 (5):1-6. doi: 10.1186/s13058-014-0442-6.
Gibbon, Sahra. 2013. “Ancestry, Temporality, and Potentiality. Engaging Cancer Genetics in Southern Brazil.” Current Anthropology 54 (7):107-117.
Jolie, Angelina. 2013. “My Medical Choice.” The New York Times, 14/05/2013.
Karanikolos, M, P Mladovsky, J Cylus, S Thomson, S Basu, D Stuckler, and M McKee. 2013. “Financial crisis, austerity, and health in Europe.” Lancet 381 (9874):1323–1331. doi: http://doi.org/10.1016/S0140-6736(13)60102-6.
Kehr, Janina. 2014. “Against Sick States: Ebola Protests in Austerity Spain.” Somatosphere Accessed 15/11/2016.
Kilshaw, Susie, Tasneem Al Raisi, and Fouad Alshaban. 2015. “Arranging marriage; negotiating risk: genetics and society in Qatar.” Anthropology & Medicine 22 (22):98-113. doi: http://dx.doi.org/10.1080/13648470.2014.976542.
Livingston, Julie. 2012. Improvising Medicine: An African Oncology Ward in an Emerging Cancer Epidemic. Durham: Duke University Press.
Lock, Margaret, and Vinh-Kim Nguyen. 2010. An Anthropology of Biomedicine: Wiley-Blackwell.
McCarthy, Mark. 2016. “Diamonds in the Dirt: Using Genetics and Genomics to Inform Biology and Treatment of Type 2 Diabetes (keynote lecture).” 6th Pan-Arab Human Genetics Conference, Dubai, 20-23/01/2016.
Modell, Bernadette, and Anver Kuliev. 1998. “The History of Community Genetics: The Contribution of the Haemoglobin Disorders.” Community Genetics 1:3-11.
Oman News Agency. 2015. “Steps taken to cut govt expenses: H E Balushi.” Muscat Daily, 29/12/2015.
Oman News Agency. 2016. “28% fall in Oman’s exports.” Muscat Daily, 6/11. Accessed 7/11/16.
Pfeiffer, J, and R Chapman. 2010. “Anthropological Perspectives on Structural Adjustment and Public Health.” Annual Review of Anthropology 39 (1):149-165. doi: http://doi.org/10.1146/annurev.anthro.012809.105101.
Rapp, Rayna. 2000. Testing women, testing the fetus. The social impact of amniocentesis in America. London: Routledge.
Reuters. 2016. “Title.” 01/01/2016.
Valeri, Marc. forthcoming, 2017. Oman. Politics and society in the Qaboos State [2nd ed]. London / New York: Hurst / Columbia University Press. Original edition, 2009.
World Health Organization. 1999. Services for the prevention and management of genetic disorders and birth defects in developing countries. Geneva: WHO.
World Health Organization. 2010. Birth defects. Report by the Secretariat (Sixty-third World Health Assembly A63/10 – Provisional agenda item 11.7). Geneva: WHO.
[1] Throughout the text, I draw attention to particular analytical categories using italics.



Human Genetics 2018 is purely an online scientific community event. This conference will mainly focus on the topics Biochemical genetics ,Cancer Genetics, Clinical Genetics, Cytogenetics, Developmental Genetics, Genetic disorders, Genomics, Genetic Counseling, Molecular genetics, Population genetics and Pharmacogenomics.
Human genetics 2018 will bring together interdisciplinary researchers working in various life science fields & lay a platform for all Academicians, Scientists, Young Researchers, Pharmacists, Genetic counselors to interact & intend their advanced scientific researches with global eminent scientists.