Drawing on participant observation of COVID-19 tests and blood donation, this article demonstrates how micro-interactions between medical personnel and laypeople can constitute trust, grounding the heavily debated topic ,trust in medicine’ in everyday life.
Trust is one of those buzzwords that rolls off the tongue and flits across magazine articles on relationship advice, that buzzes around your head like a mosquito when you’re trying to concentrate. Difficult to place, to pin down and even more difficult to tune out. In the context of the COVID-19 pandemic, trust has been a favoured buzzword, as trustworthiness of fellow citizens, of government measures and medical advice has repeatedly been questioned. Medical institutions have been called upon to inform policy, medical concepts and technologies such as herd immunity and PCR-tests have become prominent parts of our individual lives and interactions. This ethnographic essay is an attempt to capture the situational production of trust in interactions between medical personnel and laypeople, using the means of participant observation and reflexive ethnography (Ellis & Bochner 2000: 740f). By providing a specific empirical context, I aim to contribute to productive conversations on the slippery subject of trust.
During visits to a COVID-19 test site and a blood donation centre in Vienna in the spring of 2021, I came to conceive of trust as something produced through interactions: as something malleable, which waxes and wanes, rather than a binary opposition of absolute trust and absolute distrust. Sociologists and historians such as Niklas Luhmann or Steven Shapin have explained the function of trust as a fundamental social institution which reduces complexity in everyday life (Luhmann 2014, Shapin 1994). Trust allows us to depend on others, on the knowledge they have found, the technologies they have developed, the frameworks they have built. “We board a plane trusting it to get us safely to our destination not because we have familiarity with the design engineer or the pilot but because we trust that reliable systems of expertise were brought to bear in constructing the plane and will be devoted to flying it.” (Shapin 1994: 15) Akin to the aeroplane passenger, I entered my field site with a baseline of trust in medical professionals and the Austrian health care system. Such trust will vary between individuals, which is exactly why I find it productive to examine trust-creation in specific interactions. Trust in systems, characterised by Anthony Giddens as a symptom of modern complexity, entails a more abstract social relationship than trust in persons (Giddens 1995: 88). However in the case of medicine, interpersonal and system trust are interrelated. A patient’s trust in the nurse giving them an IV cannot be understood without the context of medicine as a science, as an institution, as a part of human history. But the nurse has some range of freedom, some choice as to how they behave. In this discretionary space it is up to the individual how they convey trustworthiness. Medicine as an institution can survive some of its individual representatives being untrustworthy or being distrusted, but it cannot function without any interpersonal trust at all.
A patient’s trust in the nurse giving them an IV cannot be understood without the context of medicine as a science, as an institution, as a part of human history.
COVID-19 tests are a procedure intended to create certainty. You enter as an uncertified, potentially contagious individual and leave either knowing you are ill and need to be quarantined, or with a certification of health and permission to mingle in public. Regularly testing as many people as possible can help to cut short chains of infection and slow the spread of the virus, which in turn prevents health care infrastructure from becoming overburdened. Making testing accessible benefits health care workers as well as the general population. The test centre in Vienna’s Stadthalle seemed designed to process individuals as quickly and smoothly as possible. Stern instruction-signs – “Taking pictures is forbidden in the entire test area” – hung alongside friendly banners proclaiming: “Let’s help together!” Disinfectant, scrubs, disposable protective body suits, gloves and the omnipresent FFP2 masks served the obvious purpose of preventing infection, but also helped to create the impression of a well-oiled machine. Well-known pop songs played over the sound system, interspersed with occasional reminders that FFP2 masks are mandatory. The people waiting in line would sometimes sway to the music, their minds taken off the tense wait for a result, or boring delay in their routine. At the blood donation centre, the clinical atmosphere was also dispersed by background music, and screens displaying a slideshow of “fun facts”. After giving blood, visitors proceeded to a café-like room decorated with cheerful flowers where food and drink were available free of charge for recovering donors.
Throughout my observation I identified redundancy and routinization as key factors in creating a trustworthy setting. There was a learning curve to getting Covid-tested. While early visits were full of anxiety and confusion (about the swabbing procedure itself, about the consequences of testing positive…) after a few months, the process had become no more daunting than buying groceries. For the most part I could move through the test centre on autopilot, letting my mind wander. Once I had learned to interpret the test result myself, even the waiting anxiety diminished. But ongoing slight changes in setting and routine could catch interactional partners off guard and generally undermine the trustworthiness of the setting. For instance, when the word “negative” on the paper result certificate was swapped out with “not detected”, I observed several people picking up their certificate, glancing at it and returning to ask the check-out personnel whether this meant that they had Covid or not.

Photo by World Bank Photo Collection (Flickr, CC BY-NC-ND 2.0)
What reads as trustworthy depends on context as much as the actions performed. In the test centre, which revolved around preventing infection, touch was to be avoided, distance was valuable, and friendliness extended to the phrasing of instructions and short courtesies like “Thank you” or “Have a nice day”. To some, relaxed chatting might even have seemed disconcerting or frustrating, as the goal was generally to move through each step of the testing process as quickly as possible. However, the staff at the blood donation clinic, when dealing with me as a vulnerable patient who had nearly passed out on them, showed professionalism in an entirely different way. Their humour and relaxation signalled that they had the situation under control, that there was nothing to fear. Distance would have been alienating, and small, comforting touches were reassuring. In either circumstance, trust hinged upon institutional guidelines but also micro-actions which were at the discretion of the individual.
For instance, when the word “negative” on the paper result certificate was swapped out with “not detected”, I observed several people picking up their certificate, glancing at it and returning to ask the check-out personnel whether this meant that they had Covid or not.
Both medical settings I observed had redundancies built into them. Before blood donation, I was questioned in two separate doctors’ offices about various risk factors, (Had I recently left the country? Had I been ill?), had my blood pressure measured twice in a row and was asked by each new interactional partner to repeat my name and birthdate. Redundancies seemed to be working against a slip up by distributing decisions between multiple people, and sometimes non-human actors, such as a blood pressure monitor. The latter actors are often assumed to be even more trustworthy, as they have no agenda of their own and do not lie (Weichselbraun 2019: 508).
My observation stints at the blood donation centre provided me with insights on the significance of transparency and autonomy. Patients have the right to autonomous decisions, however in medical practice this autonomy is frequently limited, because patients are reliant on expert knowledge and advice, or are incapable of formulating and communicating independent decisions (e.g. patients who are unconscious or incapacitated, small children). Doctor and medical ethicist Claudia Wiesemann presents trust as a solution to the problem of hampered autonomy. Viewing patients as trust-givers whose autonomy is to be taken seriously prevents paternalism. The patients’ personhood is respected, decisions on their welfare are not made without them, even if their autonomy is limited (Wiesemann 2016).
The staff I interacted with at the donation centre often explained what they were doing, as they were doing it. Before donating, the doctors and nurses who measured temperature and blood pressure read the numbers out loud. After I experienced a circulatory collapse on my first visit I noticed, even though I was slightly dazed, that the staff talked to me as much as they talked about me. I got to lie down behind a screen to give me some privacy until I recovered. A doctor bent down to my eye-level to explain what medication they wanted to give me to stabilise my circulation. One of the staff showed thoughtfulness by putting the medication in a cup of sweet soda to mask the unpleasant taste. Reassuring me seemed nearly as important as getting me to drink fluids and getting my blood sugar up. Routinization and institutionalisation need not preclude personal connection, instead the “personal touch” forms part of what makes the institution trustworthy, and can become part of the routine for members of the institution.
However, this doesn’t mean that the well-oiled machine never chokes. In literature on trust, a lack of trust is frequently classified as automatically negative, and a deficiency on the part of the person or parties who cannot bring themselves to trust (Baier 1986: 231f). But in the case of historically marginalised populations, the pathology does not lie with the individual who cannot trust, it lies with the system that cannot earn trust. As evidenced by the current example of vaccine hesitancy, after centuries of systemic racism, exploitation and numerous cases of misconduct against Black patients, it is unsurprising that Black Americans are more likely to question the trustworthiness of a government recommendation to vaccinate (Warren et al. 2020: 121(1), Jamison et al. 2019: 90f).
Routinization and institutionalisation need not preclude personal connection, instead the “personal touch” forms part of what makes the institution trustworthy, and can become part of the routine for members of the institution.
I believe that viewing system trust from the perspective of marginalised people can reveal where a system’s failings lie. One thing to keep in mind about reflexive ethnography and using my own experiences as a means of gathering knowledge, is that what I learn is influenced by my position in society and what interactional partners know or assume about me. My blood pressure was compared to a baseline of what is considered normal for women who are roughly my age and weight. The pre-donation questionnaire specifically addresses women with questions on pregnancy and singles out sexual relations between men as indicators of unsuitability. When I started to feel weak after donating, I began interacting with the staff from a slightly different position, as a vulnerable patient, as someone who was temporarily restricted in her autonomy. But I was also addressed by the nurses specifically as a young woman, one of them joking that they’d get me back on my feet with “Womanpower”, another assuming I had a male partner to come pick me up. Medical institutions categorise people for the purpose of efficiency. But an individual who does not fit the norm, for whatever reason, can be alienated or harmed by the standardised “one-size-fits-all” approach. This can range from minor inconveniences to very serious medical bias and neglect. For medical professionals seeking to increase trustworthiness amongst a wide variety of patients, it may be worthwhile to consider to what extent their habitual interactions accommodate or exclude persons occupying a marginalised position in society. Even patients possessing a form of privilege or who appear to fit standardised expectations at first glance may be vulnerable in less obvious ways.
Almost a year after this fieldwork, the pandemic continues to haunt us. Debates on the trustworthiness of medicine as an institution, as well as on how government policy should draw on medical expertise, rage – or buzz – on. I hypothesise that what I observed on a micro-level can to some extent be applied to a macro-level. In the context of the pandemic, trust in medicine may be hurt by short-notice and untransparent changes, like the sudden alteration of the test certificate. In contrast, more transparency in decision-making processes which lead to restrictive safety measures could potentially help alleviate the discomfort caused by hampered autonomy. Nonetheless, throughout the variety of encounters I experienced, trust presented itself as more than a simple formula of action-reaction. What constituted a trustworthy action or environment was entwined with power relations, the roles I inhabited, how I perceived others and was perceived by them. What can comfort one person may alienate another. For interactional partners in medical settings, trust remains difficult to pin down.
References
Baier, Annette (1986): Trust and Antitrust. In: Ethics, Vol. 96, No. 2 (Jan., 1986), 231-260.
Ellis, Carolyn / Bochner, Arthur P. (2000): Autoethnography, Personal Narrative, Reflexivity. Researcher as Subject. In: Denzin, Norman / Lincoln, Yvonna (eds.): Handbook of Qualitative Research 2. Edition. Thousand Oaks, 733-768.
Giddens, Anthony (1995): The Consequences of Modernity. Repr. Cambridge/Oxford.
Jamison, Amelia S. / Crouse Quinn, Sandra / Freimuth, Vicki S. (2019): “You don’t trust a government vaccine”: Narratives of institutional trust and influenza vaccination among African American and white adults. In: Social Science & Medicine 221, 87–94.
Luhmann, Niklas (2014): Vertrauen. Ein Mechanismus der Reduktion sozialer Komplexität. 5th ed. Repr. Stuttgart.
Shapin, Steven Hobbes (1994): A social history of truth. Civility and Science in Seventeenth-Century England. Chicago.
Warren, Rueben C. / Forrow, Lachlan / Hodge, David Augustin / Truog, Robert D. (2020): Trustworthiness before Trust — Covid-19 Vaccine Trials and the Black Community. In: New England Journal of Medicine. 383(22), e121(1-3).
Weichselbraun, Anna (2019): Of Broken Seals and Broken Promises: Attributing Intention at the IAEA. In: Cultural Anthropology 34, Nr. 4: 503-528.
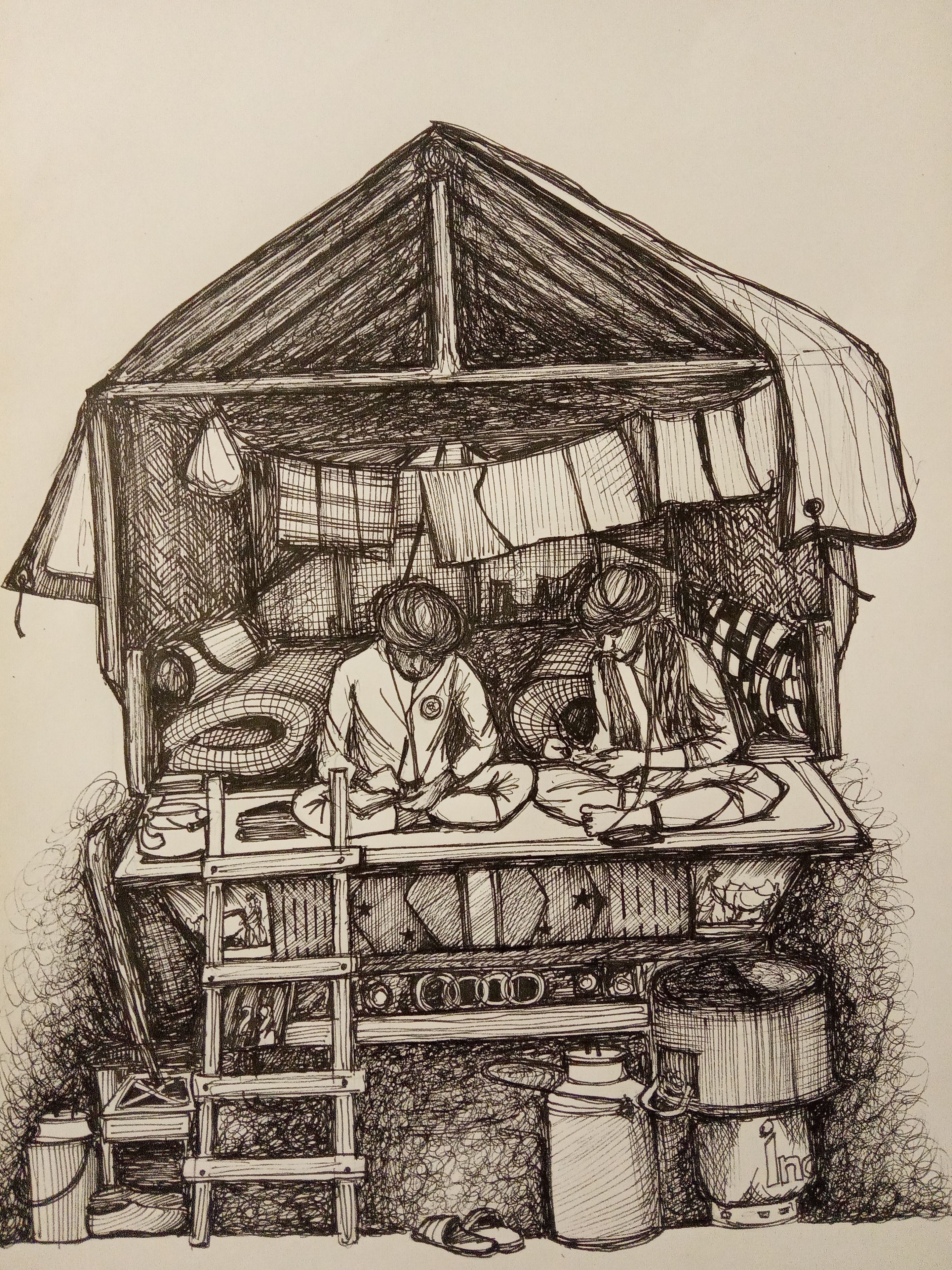
Featured image by Mat Napo on Unsplash